- Introduction
- Registration
- Log In
- Navigation
-
Eligibility Lookup
- Initiate Eligibility Lookup
- Initiate Patient Status Lookup
- Beneficiary Eligibility Information Panel
- Part B Deductible
- Medicare Advantage
- Medicare Secondary Payer
- Crossover
- Qualified Medicare Beneficiary
- Home Health Plan
- Hospice Notice of Elections
- Hospice Benefit Periods
- Inpatient and SNF Spell History
- End Stage Renal Disease
- Preventive Services
- Audiology Screening
- Hepatitis Screening
- COVID-19 Vaccine
- Flu Vaccine
- Pneumococcal Vaccine
- Cardiac Rehabilitation
- Pulmonary Rehabilitation
- Acupuncture Benefits
- Smoking Cessation Counseling
- Cognitive Assessment and Care Plan Information
- Therapy
- Diabetes Self Management Training (DSMT)
- Medical Nutrition Therapy (MNT)
- Accessing Eligibility for MDPP in NGSConnex
- Claims Status Inquiry
- Part B Claim Submissions
- Appeals
- ADR
- Inquiries
- Resources
- MBI Lookup
- Remittance
- Part A Prior Authorization Request
- Part B Prior Authorization Request
- Financials
- Manage Account
Initiate a Redetermination
Table of Contents
Initiate a Redetermination
An initial determination is communicated on the provider’s Remittance Advice. A redetermination request must be submitted within 120 days from the date of receipt of the initial claim determination.
- Select the Appeals button on the home page.

- In the Select a Provider panel, click the Select button next to the applicable provider account.

- Select Claim Search to search for the claim you are appealing.
- Enter any of the following search criteria in the filters fields.
- Medicare number
- Claim Number
- From Service Date
- To Service Date
- Select the Search button.
- Click the checkbox next to the claim you are appealing.

- Select the Initiate Redetermination button.

Redetermination Details
- Complete the required Redetermination Details fields.
- Requester’s Full Name
- Requester’s Phone - enter a valid telephone number where you can be contacted if we have a question about the request submitted.
- Reason for the Appeal - indicate the reason you are requesting the redetermination and why you do not agree with the initial claim determination.
- Late Filing Reason - If the request is past the timely filing limit you must indicate the reason you believe “good cause” exists in this field.
- Does the claim you are appealing involve Medicare Secondary Payer (MSP)? – select ‘Yes’ or ‘No’
- Select the ‘Next’ button.

Claim Lines
- In the Claim Lines section, select the claim lines you are appealing by clicking the checkbox next to the line to indicate you are appealing the claim line. If a claim line has been adjudicated and you agree with the determination the claim line should not be included in the redetermination request.
- Select the Next button.

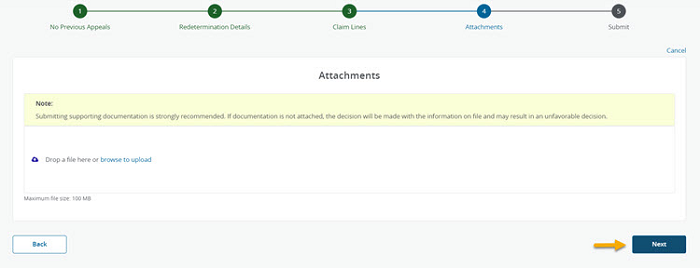
Attachments
- In the Attachments section, you will upload all supporting documentation you would like to submit with your request. You have the option to drag and drop and attachment or browse your computer for an attachment.
- We will accept most common file formats. You should submit only documentation relevant to the specific services/dates in your redetermination request and submit as few attachments as possible. You can combine multiple supporting documents in each attachments. By doing so, you will maximize the use of each attachment’s size (25 MBs) and minimize the number of attachments submitted per redetermination request. The Attachment Name should be comprised of letters and numbers. If an Attachment Name contains any special characters, you must rename the attachment.
- Select the Next button.
Submit
- Once you have verified your Redetermination request is complete and you have attached all supporting documentation, select the Submit button to transmit your request to National Government Services.

- The following message will display indicating the redetermination request was successfully submitted.
- An email verification will be sent to the email address associated with the user profile, acknowledging receipt of the redetermination request.
